The Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS) survey impacts the bottom line of home health agencies substantially, by attracting referral sources and value-based reimbursement. It is imperative that organizations understand the HHCAHPS survey, and work on improving each measure to maximize long-term growth and sustainability.
Careful Listening – Question 18
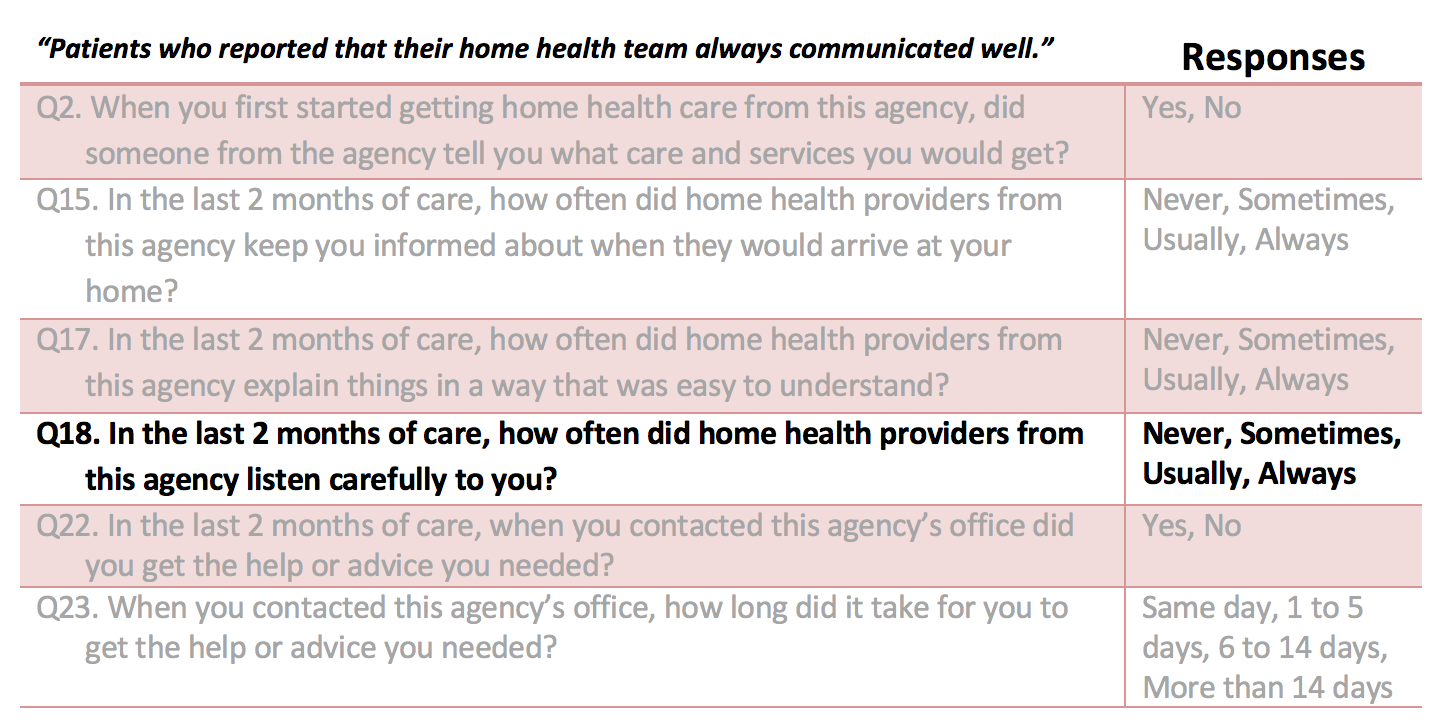
Question 18 is one of six questions included in the Home Health CAHPS survey Communications domain, designed to assess how effectively healthcare providers communicate with patients about their treatment plans.
Communications Between Providers and Patients
This question seeks to assess the patient’s perception of how frequently healthcare providers listened carefully when communicating. For optimal performance on this question, healthcare providers should not only continuously refine their listening and communication skills, but should also understand how to elicit patients’ certainty that their concerns are being heard.
Suggestions for Communications Improvement
- Ensure all staff use active listening skills when communicating with patients and caregivers/families.
- Utilize teaching aides liberally.
Active listening is indispensable in the healthcare setting. Healthcare practitioners must develop exemplary listening skills to ensure accurate patient diagnoses, safe and effective treatment, and overall provision of patient-centered care.
Cultivating effective listening skills is contingent first on understanding the distinction between hearing (passive) and listening (active). Listening is a communication proficiency requiring acquisition and continuous development- not an intrinsic capability. Healthcare professionals must conceptualize listening aptitude as an ongoing process, and organizations should equally equip staff with the necessary resources to improve these skills.
Research on patient-provider communication collectively reports favorable outcomes resulting from communication skills training, but acknowledges a lack of attention to communication training throughout the industry. A recent article on patient communication demonstrates “the lost art of listening to patients,” by referencing research findings that 30 percent of the time physicians completely overlook the patient’s reason for visiting them. Echoing sentiments from an abundance of patient-provider communication literature, the article states “it’s vital that we rekindle the skill of listening, of recognizing the emotions in the room and responding in a way that builds a trusting relationship with the patient and ultimately improves outcomes.”
AMA Listening With Empathy Module
The American Medical Association (AMA) has constructed a learning module called Listening with Empathy designed to meet the often neglected communication training needs of healthcare practitioners. Empathetic listening, as stated in the module, “allows one to be fully present for another person’s experiences,” and can improve the patient/caregiver experience, save time, and help cultivate more advantageous patient-provider relationships. The following highlights offer workable techniques to instruct agency staff and discuss institutionally.
- Employ subtle cues to convey attentive listening. Body language is a powerful indicator of whether someone is listening. Sit nearby and face the speaker to demonstrate listening. Maintain an open posture, and refrain from crossing your arms (which can often signal to the speaker that you are closed off or dismissive). Make eye contact, nod your head as appropriate, and emulate the speaker’s emotional intensity with your expressions. Periodically repeat or summarize the speaker’s communication to further signal that you are listening and understanding the information being expressed.
- Remain present when listening to the patient/caregiver. Eliminate outside distractions (e.g., phone, alarms, computer screen, and patient charts). Extend undivided attention to the speaker, particularly during the first moments of the visit when patients and caregivers are likely to provide key information upfront.
- Listen for underlying feelings, needs, or values. Watch for non-verbal indicators of feelings (e.g., body language or facial expressions). Invite the patient’s elaboration of concerns or feelings by pausing appropriately during conversation, and listen for cues that the patient is done speaking before considering verbal response. Cues can include a decrease in emotional intensity, a deep sigh, or an extended pause in the speaker’s dialogue. Remember that any verbal responses at this point should remain reflective and exhibit your continued focus on the patient’s or caregiver’s communication.
Investing in the development of communication and interpersonal skills is essential for institutions and professionals across the healthcare continuum.
Check our blogs for the series on improving your agency’s HHCAHPS scores by systematically reviewing each of the HHCAHPS questions and sharing opportunities for improvement.