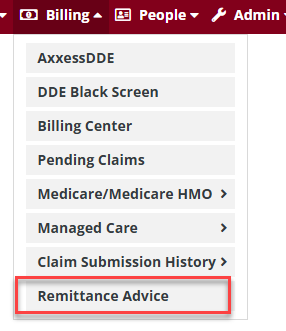
To access the Remittance Advice click on Billing->Remittance Advice
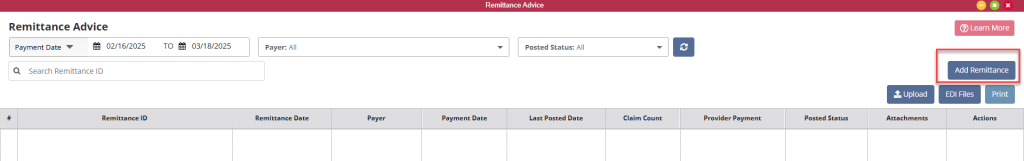
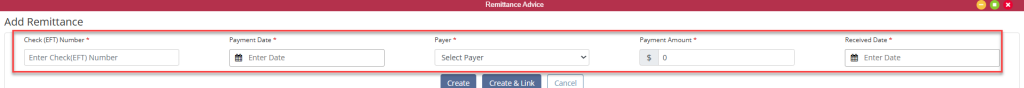
Remittance Advice pull into the Home Health solution for all agencies which are set up to bill electronically through Axxess. The Remittance Date parameter is set to a 60 day time frame prior to the current date. The user may change the date range if desired. Users who either choose not to electronically bill through Axxess or who are not yet linked may upload their Remittance Advice into Axxess. This is accomplished through the Add Remittance button in the upper middle portion of the page. Once uploaded, the user will have the same functionality as remittances that come directly into Axxess.
*Note on uploaded Remittance Advice: If wishing to post payments from the Remittance Advice seven items must be fulfilled:
Select Create or Create & Link.
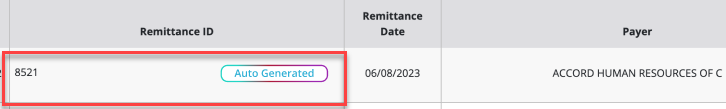
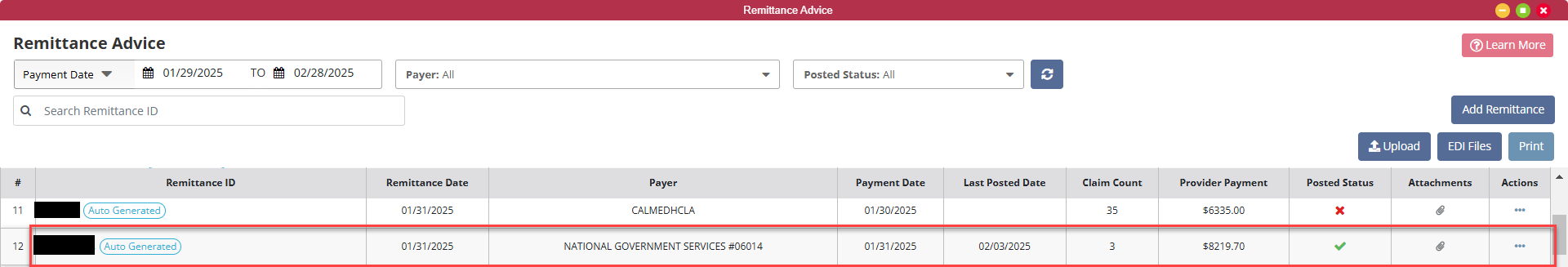
There are nine columns to the remittance file listings. First will be the Remittance ID. This is the ID associated with the payment. When viewing the Remittance ID there will be a gradient border around all the “Auto Generated” Remits, which are remits that have been automatically upload from Axxess RCM or standard border for manually uploaded remittance.
Next is the Remittance Date, the Payer, the Payment Date the organization can expect payment, the Last Posted Date, the number of claims contained in the Remittance Advice (Claim Count), the payment amount (Provider Payment), Actions, Attachments and Posted Status columns.
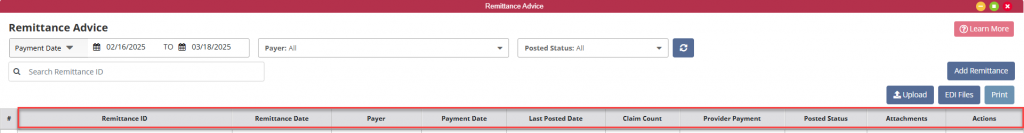
The Actions column contains two actions: View Details and Delete.
The Delete action item will delete the remittance advice from the list.

Select View Details to open the remittance advice to allow the user to view the details and post payments to the patient’s claim.
Mark as Posted does not automatically post payments within the selected remittance but indicates that remittance advice has been posted by turning the red X in the the Posted Status column to a green check mark.
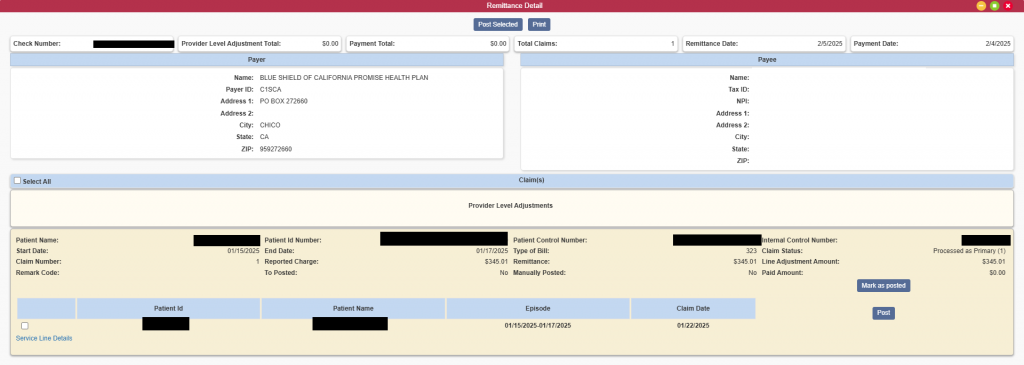
The Remittance Advice summary information pulls over to the remittance detail for quick review by the user. Below the summary are the Payer and Payee information.
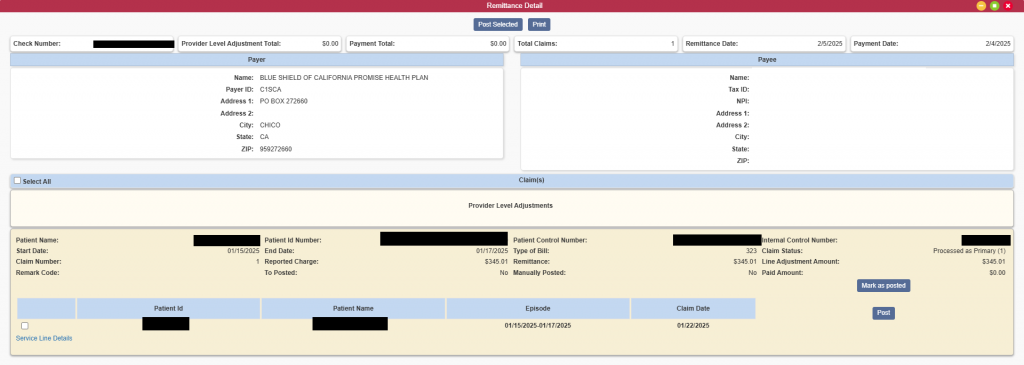
Located below the Payer and Payee information is the listing of the claims associated with the remittance advice. In addition to the Patient Name and Medicare Number, each claim line item includes:
There are several ways to post claim payments within Axxess Home Health.
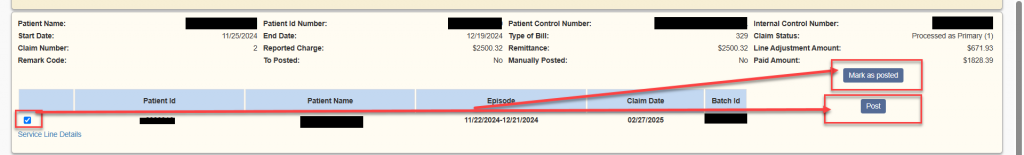
An individual claim payment may be posted by selecting the box to the left of Patient ID then selecting the Post button in the claim information or Mark as Posted selection if payment has been manually posted by user.
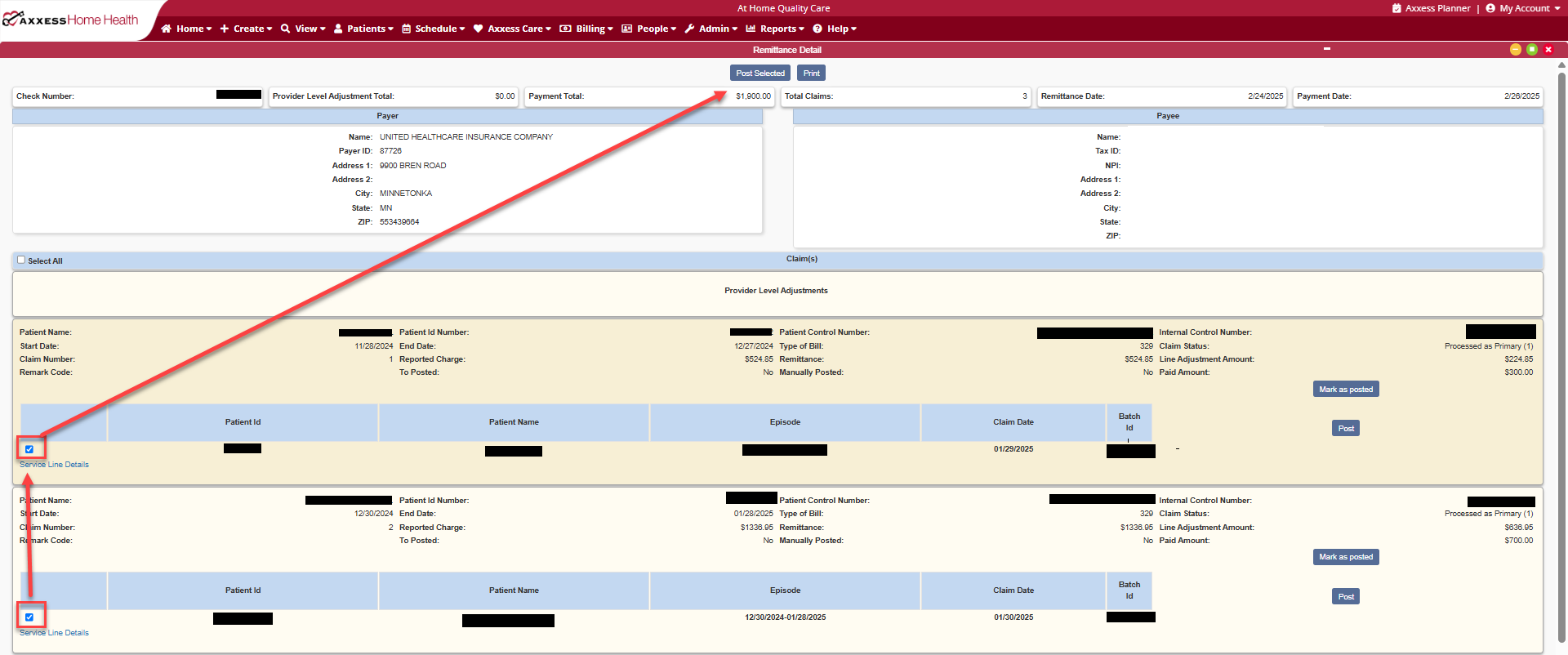
For multiple claim payment posting, select the check box within the claim information and select Post Selected at the top of the remit.
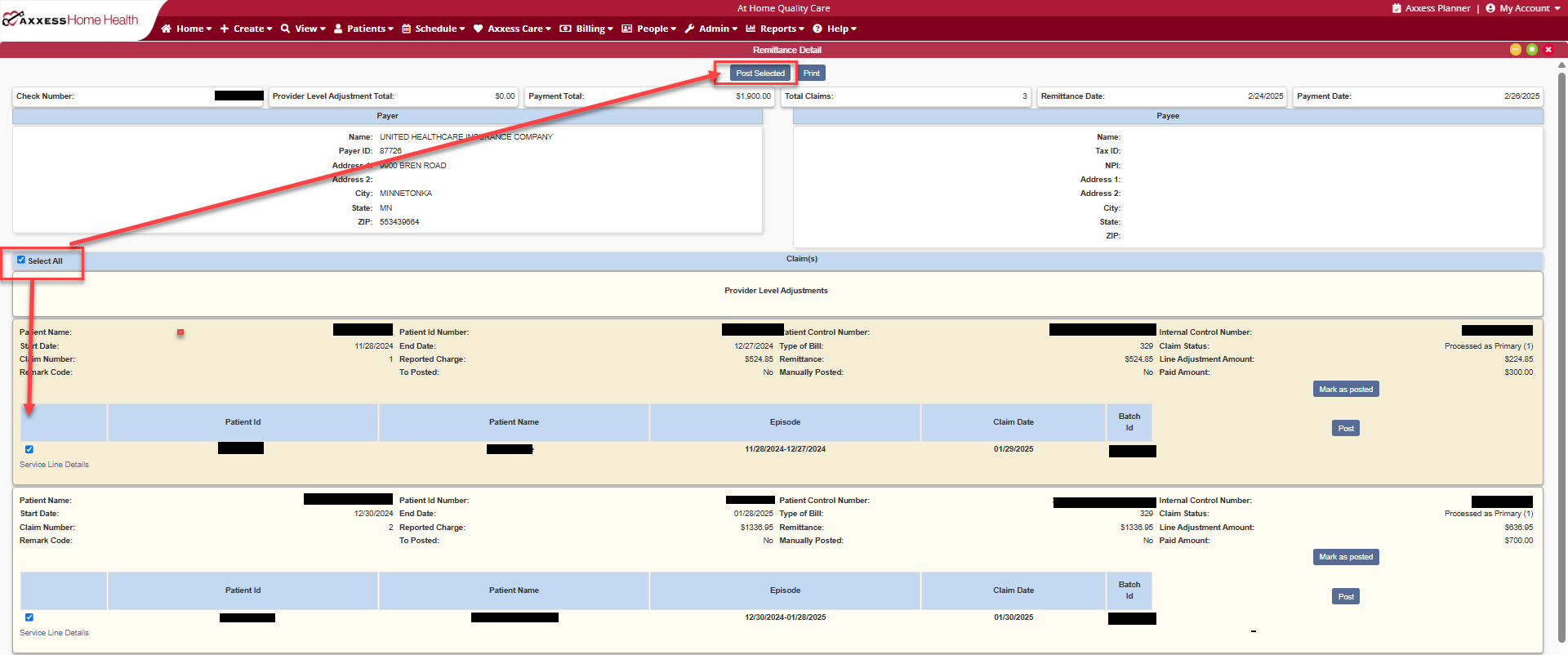
For the entire remit, select Select All at the top of the remit claim details which will put a check mark next to each claim within the remit and select Post Selected at the top of the remit.
The selection and Post button no longer appears once the payment has been posted for the claim. Claim information and posting may be viewed through the Billing Claims History for the patient.