

A comorbidity adjustment is one of four primary components that comprise the PDGM regulations effective January 2020. When an agency assesses a patient under PDGM, all diagnoses will be taken into consideration to determine whether the patient is eligible for a low or high comorbidity adjustment, if any.
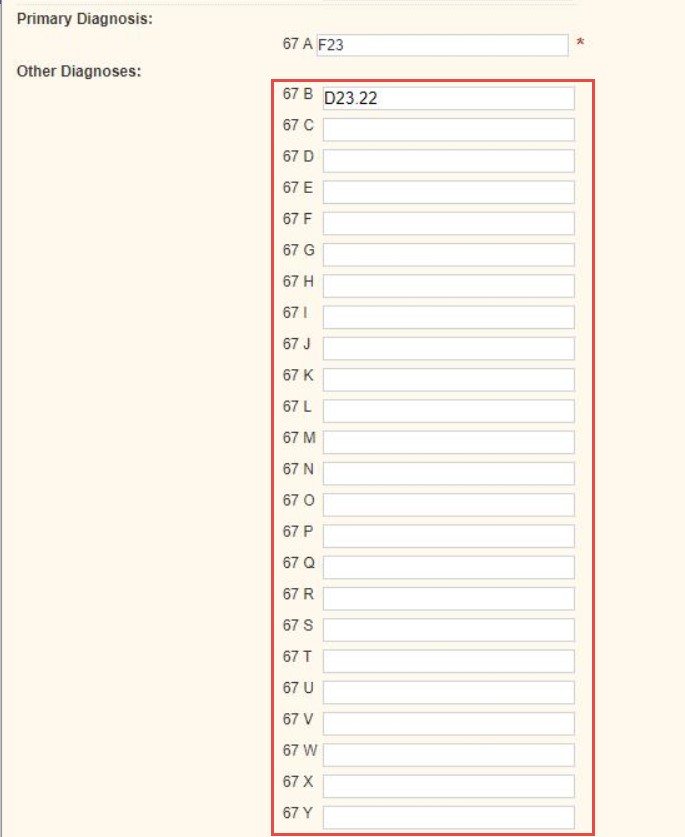
When a Medicare or Medicare HMO claim is selected for any patient, only the primary diagnosis is required, but users can also enter up to 24 additional diagnoses in the first step of the claim creation process.
With the ability to provide all diagnoses that apply to a patient’s episode of care, agencies are better equipped to:
Additional information on PDGM can be found in the PDGM section of the Help Center and in the Axxess PDGM Resource Center.