Organizations with an active Axxess RCM subscription can now validate managed care claims in Axxess Home Care using Axxess intelligence™ in the final step of the claim verification process. This innovative tool enables users to identify, review and address potential claim rejections in advance. This supports the submission of cleaner claims and fewer rejections, resulting in faster turnaround times in accounts receivable.
Claims can be opened in two ways.
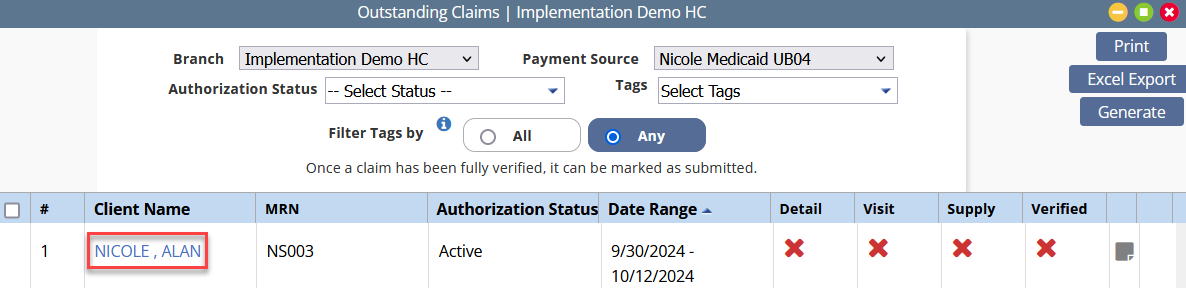
Option one: Navigate to Managed Care/Other Insurances under the Billing tab, select Outstanding Claims and navigate to your desired client.
Billing tab ➜ Managed Care/Other Insurances ➜ Outstanding Claims ➜ Select a client
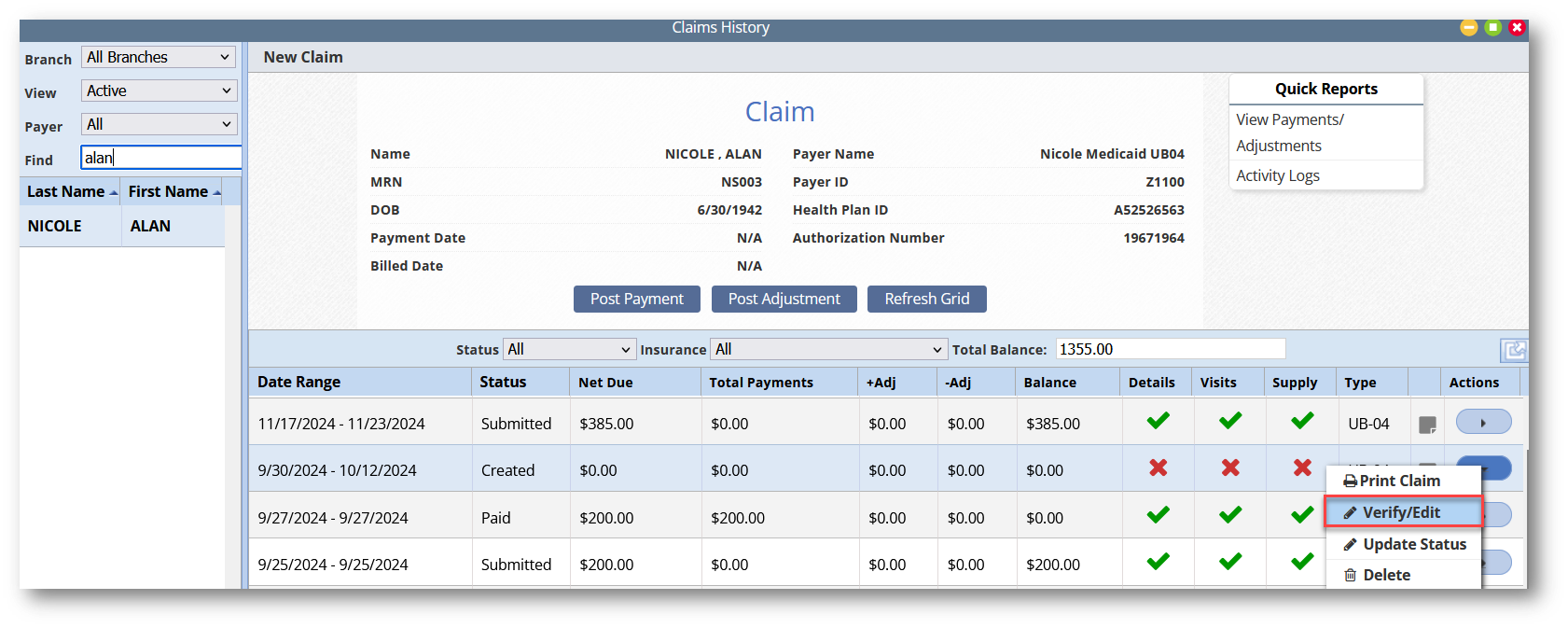
Option two: Navigate to Managed Care/Other Insurances under the Billing tab, select Claims History.
Billing tab ➜ Managed Care/Other Insurances ➜ Claims History
On the Claims History screen, search your desired client, navigate to the Actions column and select Verify/Edit.
Claims History ➜ Search client ➜ Actions ➜ Verify/Edit
Once the claim has been verified, select Complete. This will initiate claim validation using Axxess intelligence™. If an error is returned, a message will display in the top-right corner.
