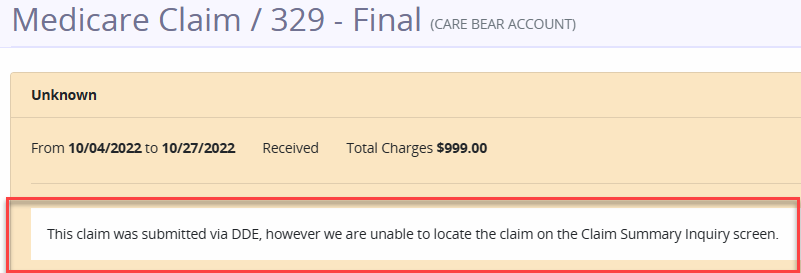
Axxess DDE now provides an Unknown Claims section that enables users to view claims marked as unknown. This enhancement streamlines operations and improves efficiency by enabling users to quickly identify claims that may not appear in the Medicare claim inquiry system.
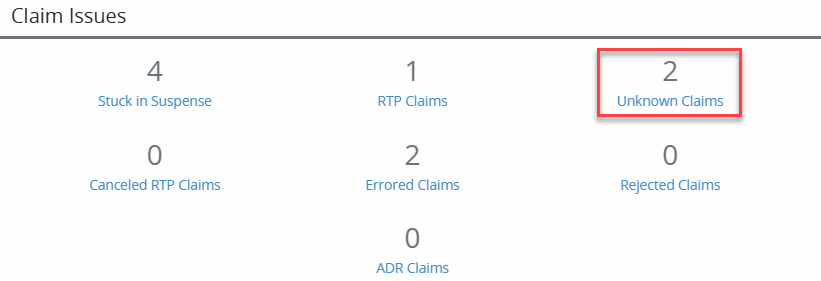
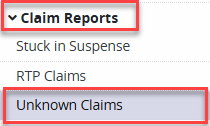
To view an unknown claim, navigate to the Claim Issues section and select Unknown Claims, or select Claim Reports under the Reports tab and click Unknown Claims.
Claim Issues section ➜ Unknown Claims
Reports tab ➜ Claim Reports ➜ Unknown Claims
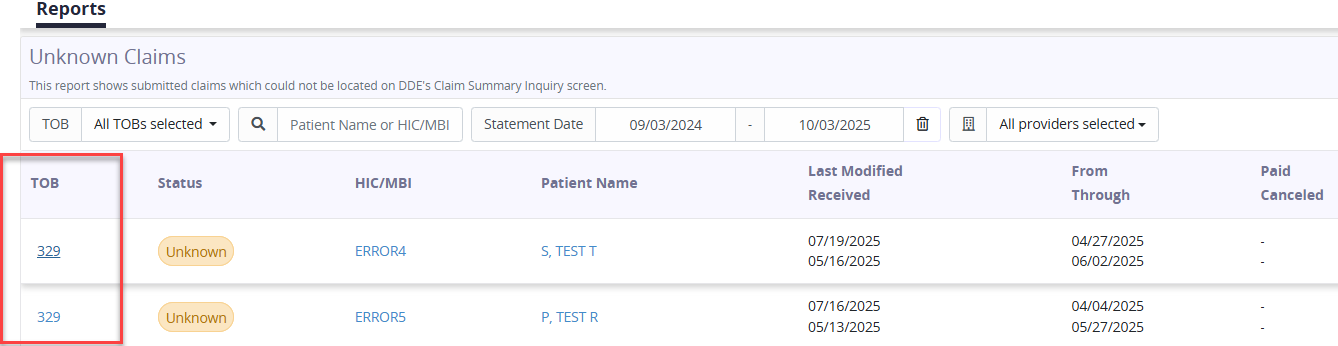
Select TOB to view the reason the claim is in the Unknown Claims section.
Updated on 12/04/2025