Through a series of automations powered by Axxess intelligence™, Axxess Hospice automatically generates the Notice of Election (NOE) and Notice of Transfer and Revocations (NOTR) based on specific user actions, eliminating the need for a manual generation process for these important documents.
Axxess enables organizations to streamline claims processing for accurate and timely claims submission to protect revenue through the Billing tab.
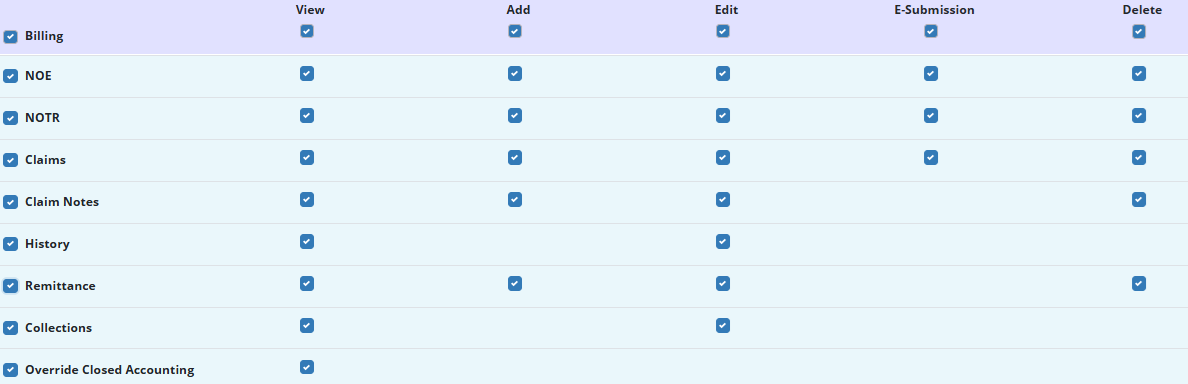
Billing features are permission-based in Axxess Hospice.
Billing permissions can be enabled when creating a new user or by editing an existing user.
To grant billing permissions to an existing user, edit the user and navigate to the Permissions tab. Scroll to the Billing section and check the boxes next to the appropriate permissions.
People tab ➜ People Center ➜ Edit ➜ Permissions tab ➜ Billing section
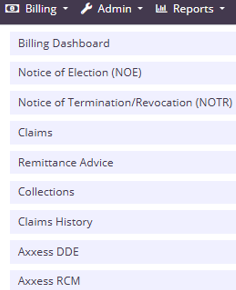
The Billing tab in Axxess Hospice includes the following menu items:
Claims displays the readiness and details of claims sorted by patient.
Claims History displays submitted claims sorted by patient.
Notice of Election (NOE) displays recently admitted patients who are in Active status in the software.
Notice of Termination/Revocation (NOTR) displays patients who were recently discharged live and are in Discharged status in the software.
Remittance Advice displays remittance advice for all payers. On this screen, users can search by Electronic File Transfer (EFT) number or date range.
Organizations with subscriptions to Axxess DDE and/or Axxess RCM will also see the respective links in the Billing tab.
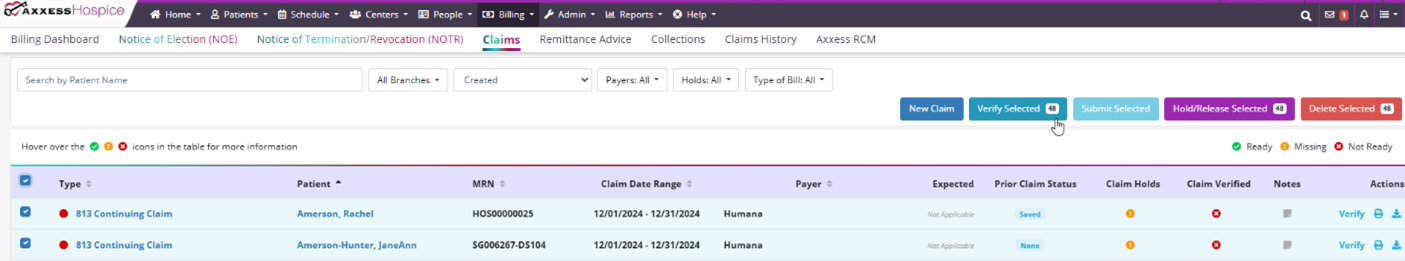
The Claims page shows claims that are pending verification and/or submission. Claims are listed with the following information:
Type of Bill
Patient – Click on the patient’s name to navigate to the patient’s chart
MRN
Claim Date Range
Payer
Expected Amount
Prior Claim Status
Claim Holds
Claim Verified
Notes
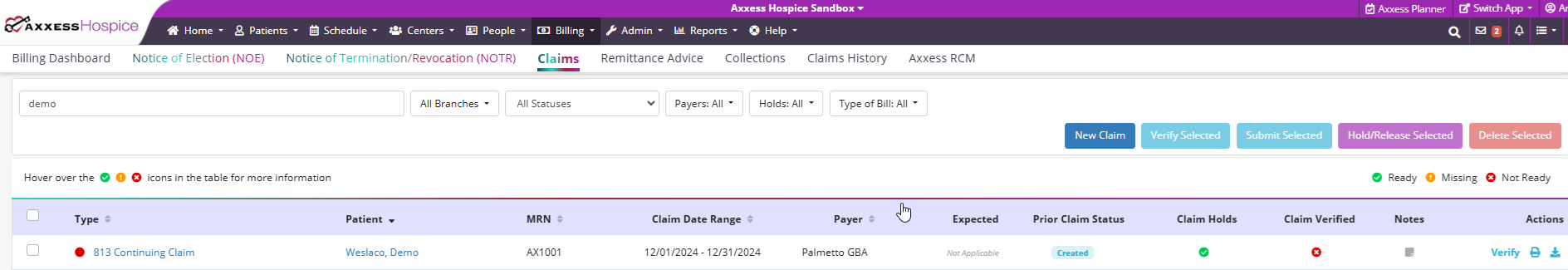
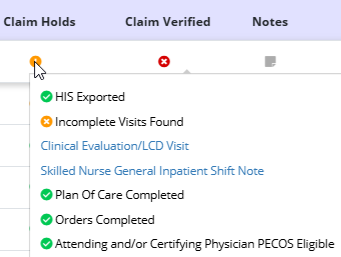
Axxess intelligence™ generates claims and checks each patient’s chart to ensure that all visits and orders within the claim date range are completed.
This information is housed under the Claim Holds icon. When clicked, users can view a list of items that may be required prior to billing a claim.
Once all information is entered, click Verify.
Once verified, a green check mark appears in the Claim Verified column. Click Submit to submit the claim to the patient’s payer.
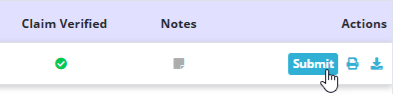
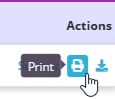
The print and download icons enable users to print and download claims as documentation.
Batch billing enables organizations to verify or submit multiple claims simultaneously.
To bulk verify claims, select the check box left of the claim and click Verify Selected. This verification process can take several minutes. Users will receive a notification message in their inbox when verification has been completed.
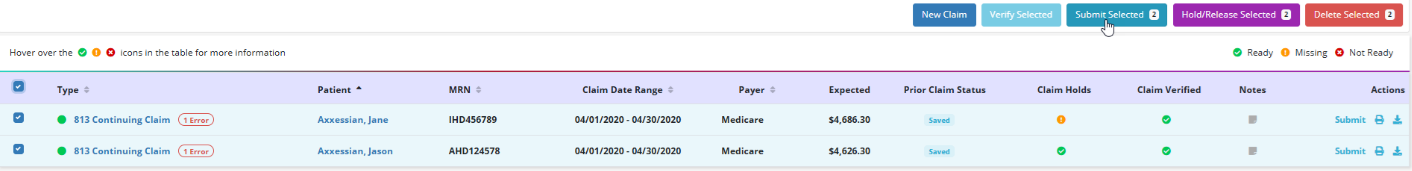
Once claims have been verified, users can submit multiple in a single batch. To submit multiple claims in a single batch, navigate to the Claims page.
Billing tab ➜ Claims
Check the boxes next to desired claims and click Submit Selected in the top right corner of the Claims screen.
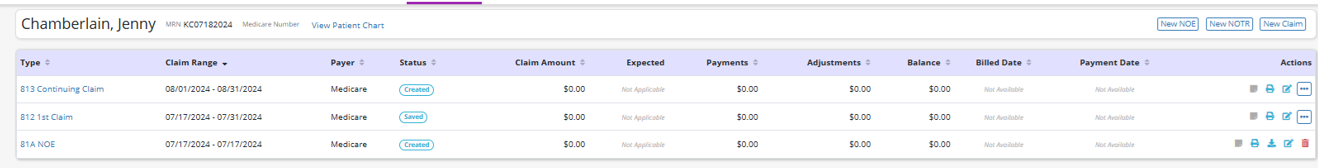
Select Claims History under the Billing tab to view a list of the following information:
Type of Bill
Claim Range
MRN
Claim Date Range
Payer
Status
Claim Status
Expected Amount
Payments
Adjustments
Billed Date – When the claim was submitted
Payment Date – When the claim was paid
Find claims for specific patients using the following filters on the left side of the screen:
Search type a patient’s name and the list narrows down as you type.
Branch select a specific organization branch (if more than one).
Status select Active, Discharged, Pending, Non-Admitted or Deceased.
Level of Care select Routine Home Care, Respite Care, Continuous Care or General Inpatient Care.
Once a patient has been selected, view the NOE, NOTR, or claim by selecting the respective hyperlink on the left side of the screen. Create a new NOE, NOTR, or claim by selecting the appropriate button in the top right corner of the screen.
Download, print, or delete billing items by selecting the corresponding icons under Actions. To navigate to the patient’s chart, select View Patient Chart in the header next to the patient’s Medicare number.
Select Notice of Election (NOE) under the Billing tab to view a list of the following information:
Days Remaining
Type of Bill
Patient Name – click on the patient’s name to navigate to the patient’s chart.
Admission Date
Election Form
Certificate of Terminal Illness
Initial Assessment
NOE Verified
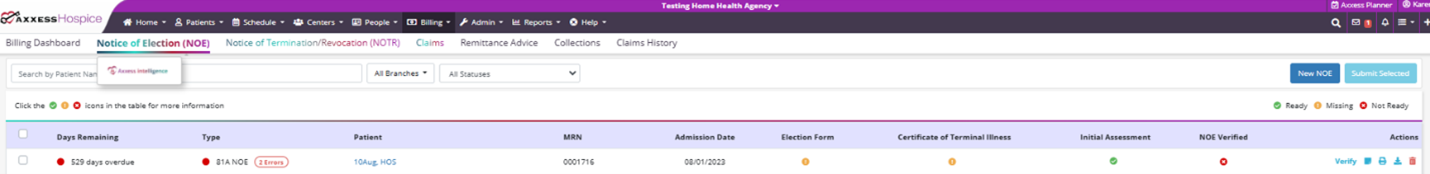
When a patient changes from Pending to Active status, Axxess intelligence™ automatically generates a Notice of Election and checks the patient’s chart to ensure that all required documents have been completed.
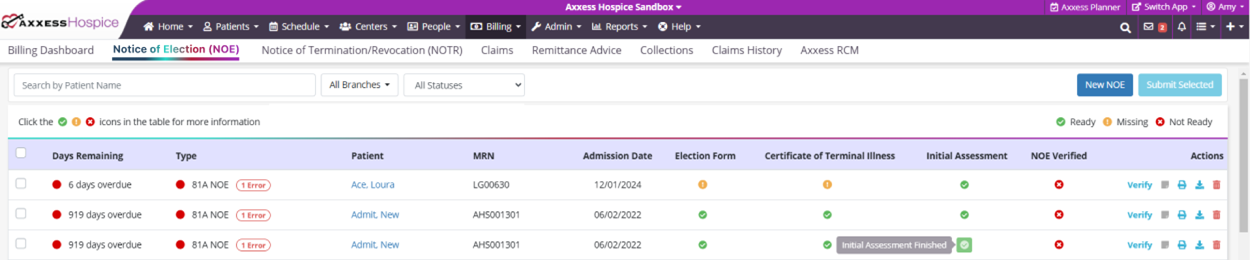
NOEs are ready in the software once each column on the NOE screen has a green check mark. To verify an NOE, select Verify under Actions and confirm that all information is correct.
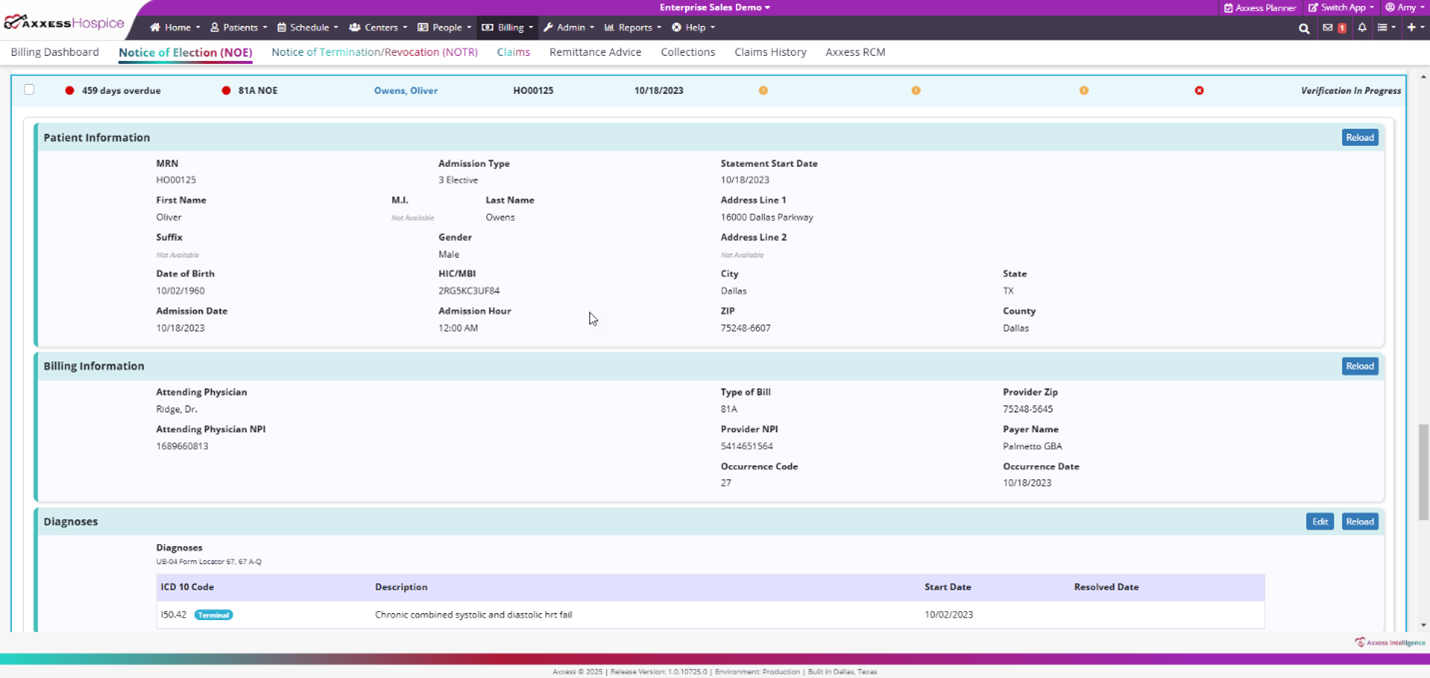
Once all information is entered and accurate, select Verify. Once verified, a green check mark appears in the Claim Verified column. Click Submit to submit the NOE to the patient’s payer.
The print and download icons enable users to print and download NOEs as documentation.
Select Notice of Termination/Revocation (NOTR) under the Billing tab to view a list of the following information:
Type of Bill
Patient Name – click on the patient’s name to navigate to the patient’s chart.
MRN
Revocation/Discharge Date
Discharge Visit
Revocation Statement
NOTR Verified

When a discharge visit or unattended discharge note is scheduled for a patient, Axxess intelligence™ automatically generates an NOTR and checks each patient’s chart to ensure that all required documents are completed.
NOTRs are ready in the software once each column on the NOTR screen has a green check mark. To verify a NOTR, select Verify under Actions and confirm that all information is correct.
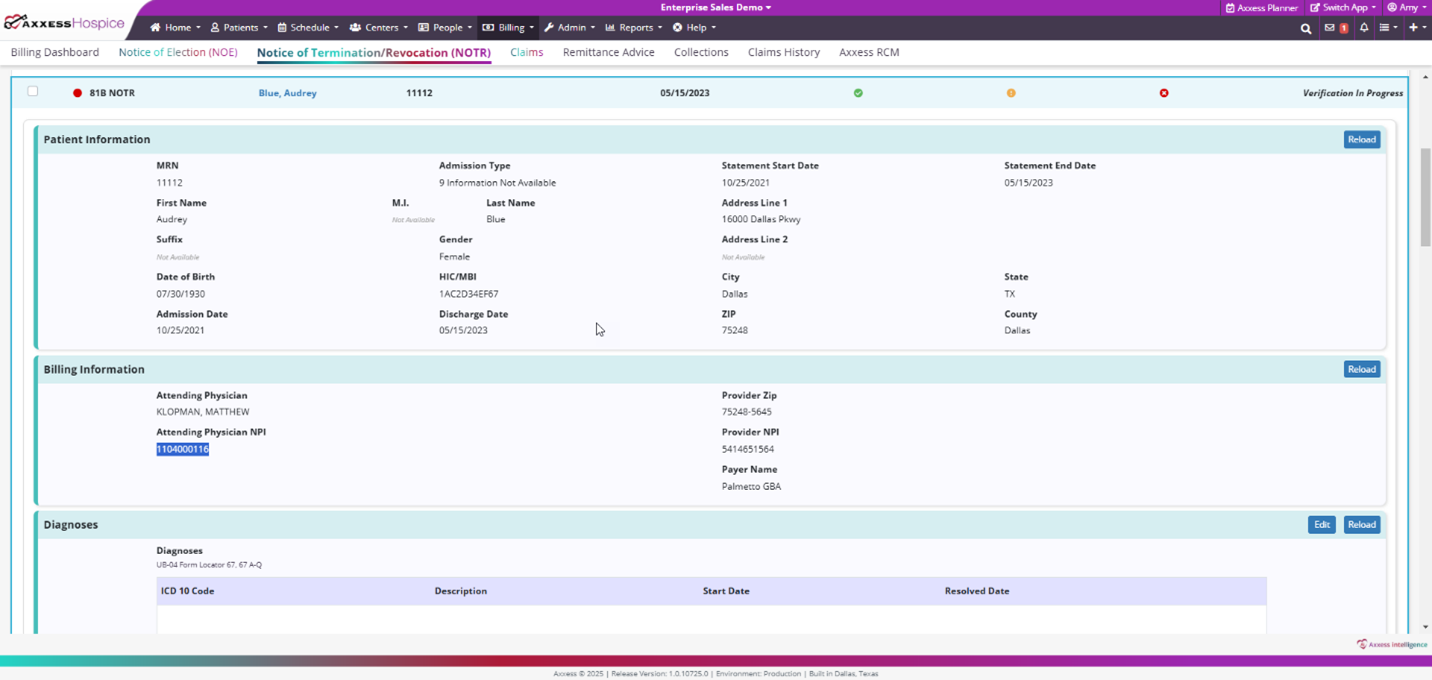
Once all information is entered and accurate, select Verify. Once verified, a green check mark appears in the Claim Verified column. Click Submit to submit the NOTR to the patient’s payer.
The print and download icons enable users to print and download NOTRs as documentation.
Select Remittance Advice under the Billing tab to view a list of the following information:
EFT Number
Payment Date
Payment Amount
Remaining Balance – outstanding amount not posted to a specific claim.
Number of Claims
Received Date
Deposit Date
Payer Name
Reference ID
Payee Name
Provider NPI
Provider Tax ID
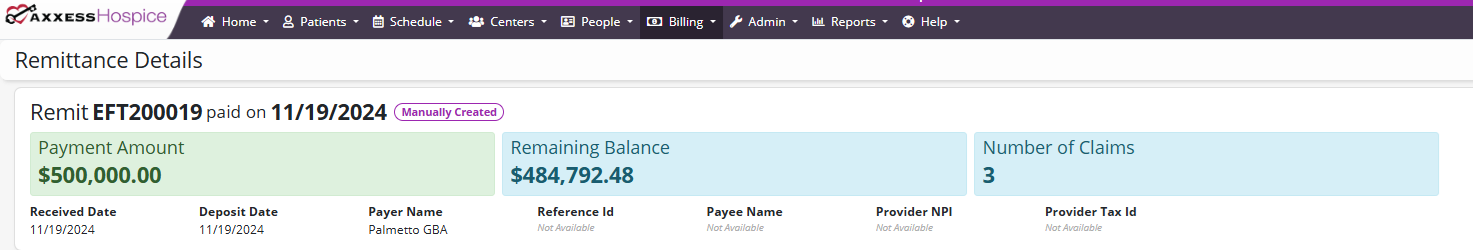
Users can search the list of remittances by EFT number or date range.
Below these details, claims linked to the remittance advice are listed with the following information:
Patient Name
Patient Control Number
Payer Claim Control Number
Type of Bill (TOB)
Statement From Date
Statement to Date
Received on Date
Claim Amount
Payment Amount
Balance
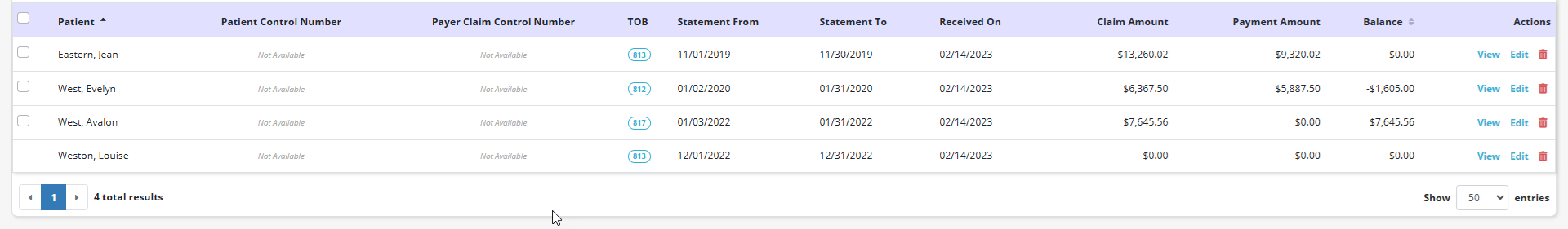
For remittances with remaining balances, users can select claims and click Auto-Adjust to automatically post payment amounts to the selected claims. To link additional claims to a remittance, select Link Claims and a list of available claims will appear for linking to the remittance. Each claim on a remittance can be viewed and edited using the buttons in the Actions column.