Routine Home Care (RHC) visits performed by telehealth must meet the patient’s needs identified in the Plan of Care, and members of the hospice interdisciplinary team must document how the patient’s needs are being met during care performed through telehealth.
Axxess has created telehealth notes for each discipline and non-discipline-specific notes to enable seamless documentation of telehealth visits for all members of the hospice team.
This functionality streamlines documentation of care provided by telehealth, and facilitates compliance with the CARES Act and CMS regulations for telehealth visits.
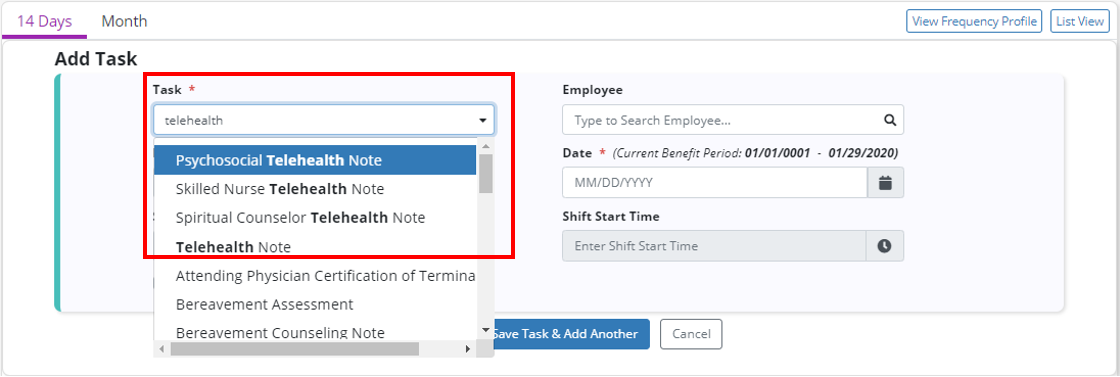
To schedule a telehealth note in Axxess Hospice, navigate to the Patient or Employee Schedule under the Schedule tab. Add a task and select the desired telehealth note from the Task drop-down menu. The following notes are available for documenting care provided by telehealth:
| Telehealth Note: Used to document general care provided by telehealth |
| Skilled Nurse Telehealth Note: Used to document nursing-specific care provided by telehealth |
| Psychosocial Telehealth Note: Used to document psychosocial-specific care provided by telehealth |
| Spiritual Counselor Telehealth Note: Used to document spiritual-specific care provided by telehealth |
Enter the remaining task details and click Save Task to save the task or Save Task & Add Another to continue adding tasks to the schedule.
Schedule tab ➜ Patient/Employee Schedule ➜ Add Task ➜ Select a telehealth note in the Task menu ➜ Complete remaining fields ➜ Save Task
The existing Telehealth Note has been updated with the following enhancements to facilitate seamless documentation of care provided through telehealth:
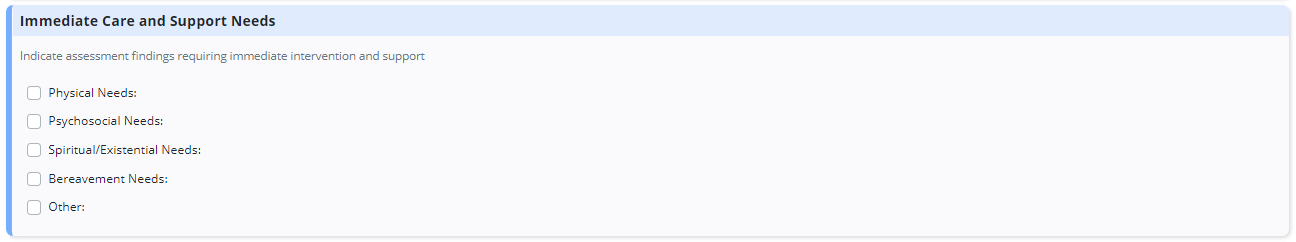
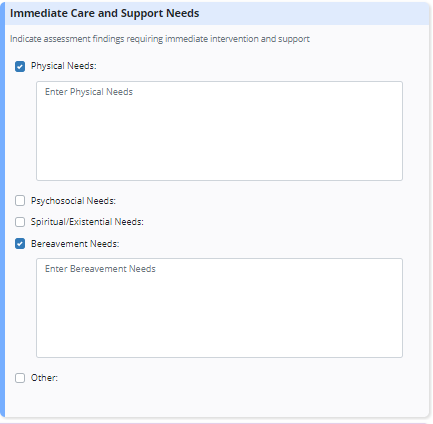
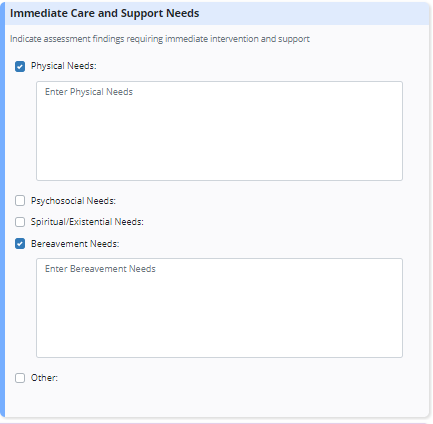
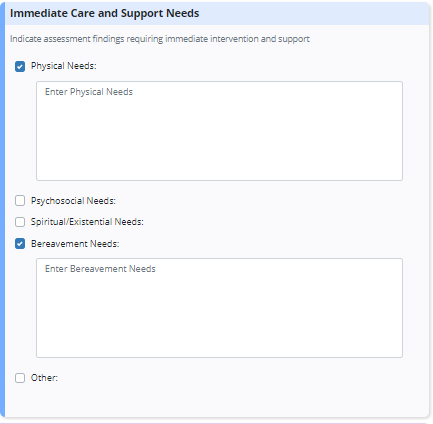
Immediate Care and Support Needs: This new section enables documentation of identified needs for the patient and family.
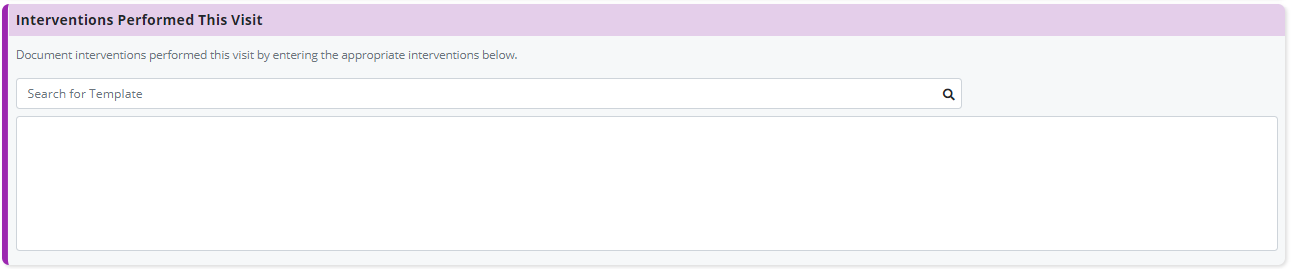
Interventions Performed This Visit: This new section enables documentation of specific care plan interventions carried out through telehealth.
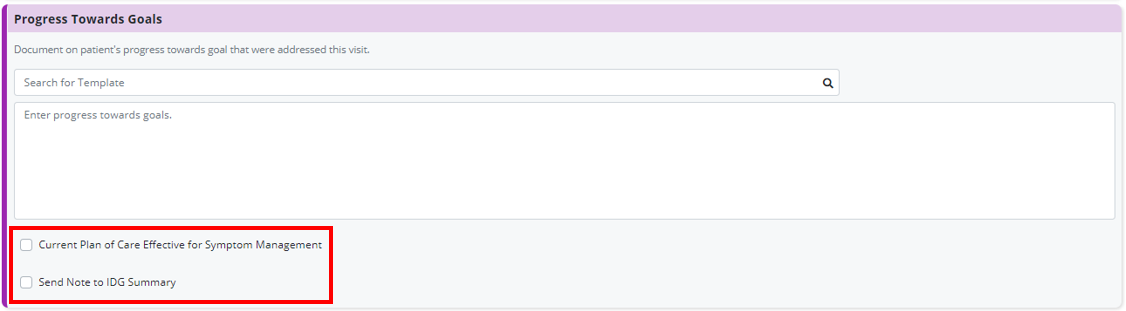
Progress Toward Goals: This new section enables documentation of the patient’s progress toward meeting the goals outlined in the Plan of Care. Similar to other documents in Axxess Hospice, documentation here can be sent automatically to the patient’s IDG summary. Click Send Note to IDG Summary to mark this documentation to flow to IDG.
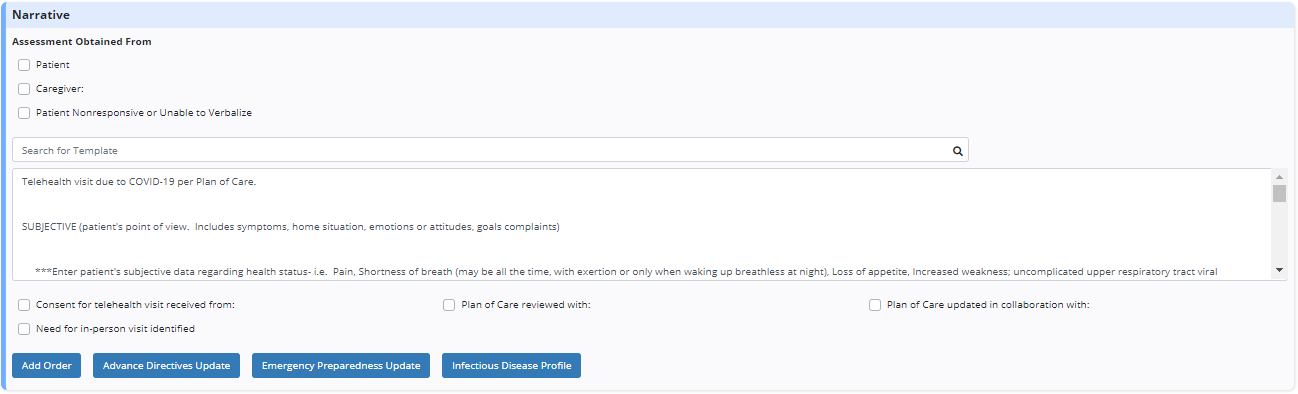
Narrative: This section has been enhanced so clinicians can document who they obtained assessment data from, who they obtained consent from for the telehealth visit, who they reviewed the Plan of Care with, and who they collaborated with to update the Plan of Care. If the need for an in-person visit is identified during the telehealth encounter, users can check the respective box toward the bottom of the section to document and address the need for an in-person visit.
New orders and changes to the patient’s Plan of Care can be documented directly from the visit note and will flow automatically to the patient’s IDG summary.
Select the Infectious Disease Profile button to add and complete a COVID-19 screening for the patient during the visit.
The Skilled Nurse Telehealth Note enables users to document nursing-specific needs of the patient during a telehealth encounter. In addition to existing telehealth note features, the following sections are included in the Skilled Nurse Telehealth Note:
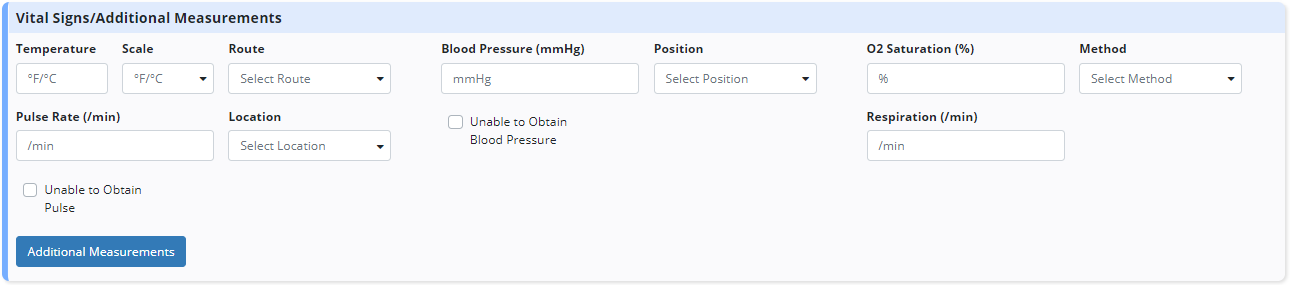
Vital Signs/Additional Measurements: This section enables users to document vital signs collected during the visit for patients who have in-home monitoring equipment or in-home caregivers who can obtain vital sign readings.
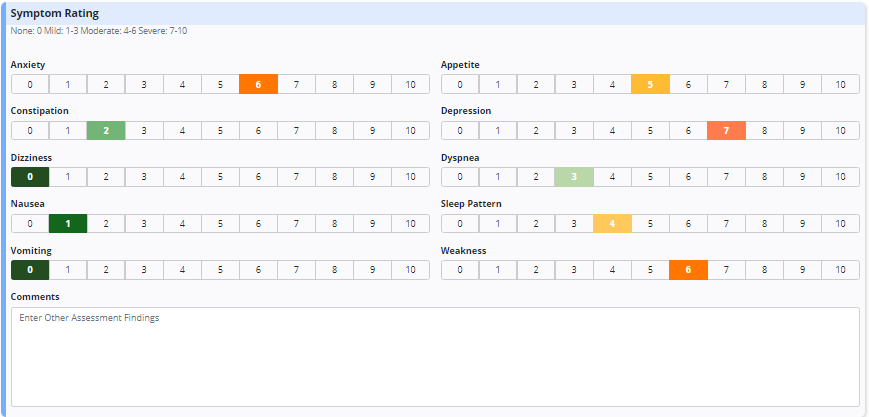
Symptom Rating: This section assists nurses with collecting subjective assessment data for key symptoms affecting the patient. Responses can be easily reviewed and monitored between visits to assess how the patient’s symptom control is improving or deteriorating.
Immediate Care and Support Needs: This section enables nurses to document the patient’s identified needs holistically, including physical, psychosocial, spiritual/existential and bereavement needs.
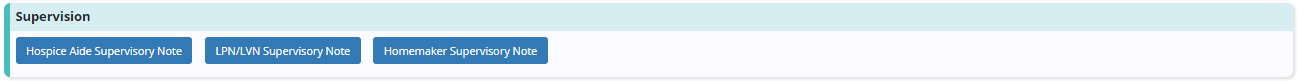
Supervision: This section provides buttons that enable users to complete a Hospice Aide, LPN/LVN, and/or Homemaker Supervisory Note directly from the SN Telehealth Note.
The Psychosocial Telehealth Note enables users to document the patient’s psychosocial and emotional needs during a telehealth encounter. In addition to existing telehealth note features, the following sections are included in the Psychosocial Telehealth Note:
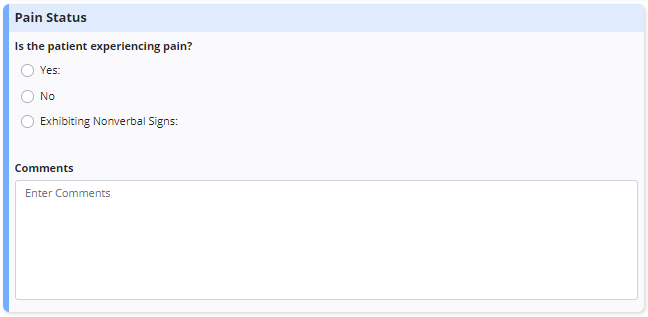
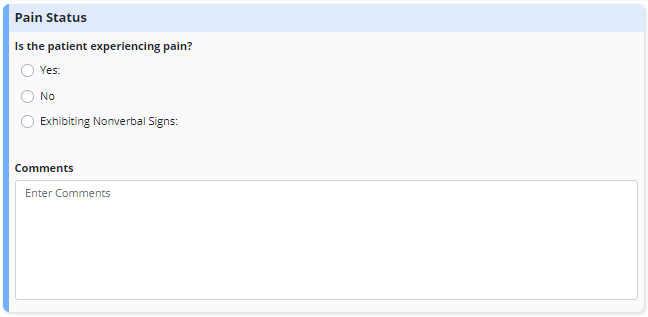
Pain Status: This section enables social workers to document brief assessments of the patient’s pain status and any communication with other members of the care team.
Immediate Care and Support Needs: This section enables social workers to document the patient’s identified needs holistically, including physical, psychosocial, spiritual/existential and bereavement needs.
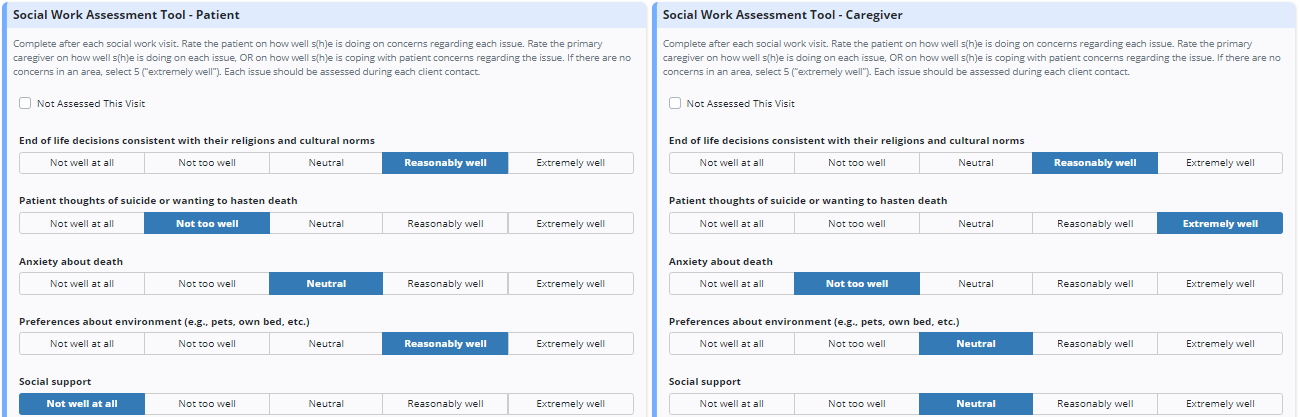
Social Work Assessment Tool (SWAT) for Patients and Caregivers: These sections enable social workers to collect measurable data about the patient’s or caregiver’s psychosocial symptoms. Based on the responses entered, the software automatically calculates a score that can be monitored over time to determine how the patient’s and caregiver’s psychosocial needs are being impacted.
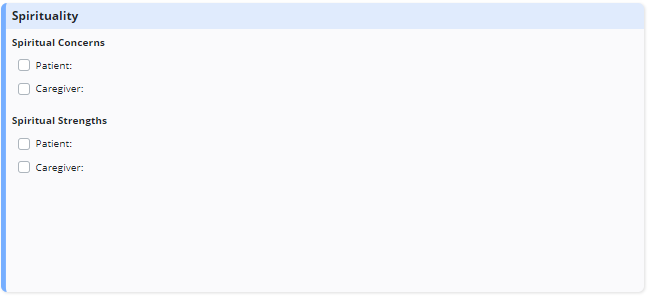
The Spiritual Counselor Telehealth Note enables users to document the spiritual needs of the patient and caregiver during a telehealth encounter. In addition to existing telehealth note features, the following sections are included in the Spiritual Counselor Telehealth Note:
Pain Status: This section enables spiritual counselors to document brief assessments of the patient’s pain status and any communication with other members of the care team.
Immediate Care and Support Needs: This section enables spiritual counselors to document the patient’s identified needs holistically, including physical, psychosocial, spiritual/existential and bereavement needs.
Spirituality: This section enables spiritual counselors to document the patient’s and caregiver’s spiritual strengths and concerns, and tailor care to meet assessed spiritual needs.