Axxess Home Health now provides OASIS-E1 assessments on both the web platform and mobile application. This enhancement facilitates compliance by aligning with the latest CMS updates, improves ease of use with streamlined visit information entry and streamlines operations by updating therapy evaluations and adding therapy discharge directly within the assessments.
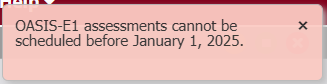
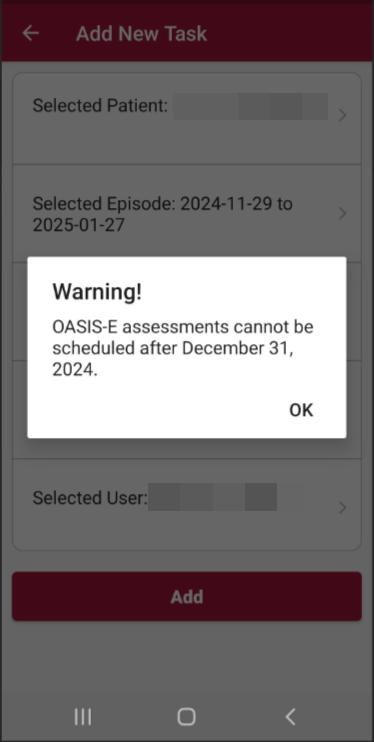
Users with the Schedule Visits/Activities permission can schedule these assessments in the Schedule Center, Quick Employee Scheduler or through the mobile application. Please note that the schedule date for these assessments should be on or after January 1, 2025. OASIS-E can no longer be scheduled after December 31, 2024. When trying to schedule one of these assessments outside of the listed dates, the user will receive an error message.
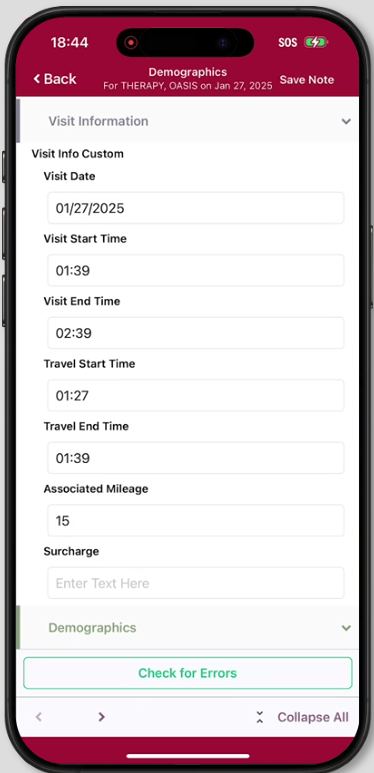
Visit Information
Users can now add visit information within the assessment prior to completion. This section is located in the Demographics tab of the Start of Care, Resumption of Care, Recertification, Other Follow-Up, Discharge, and Death at Home visit notes. This section is not a required field within the assessment, and all time validations will be flagged when the user signs and completes the note, like the current OASIS-E functionality.
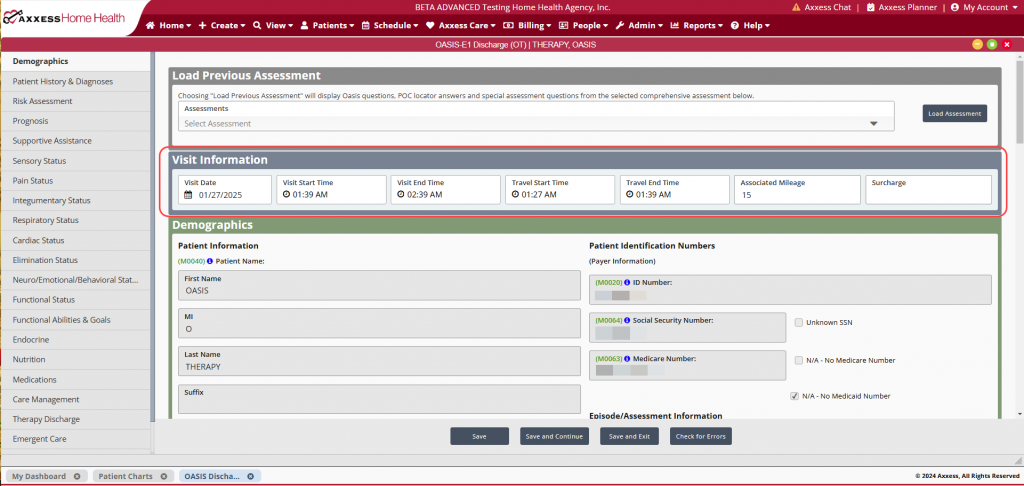
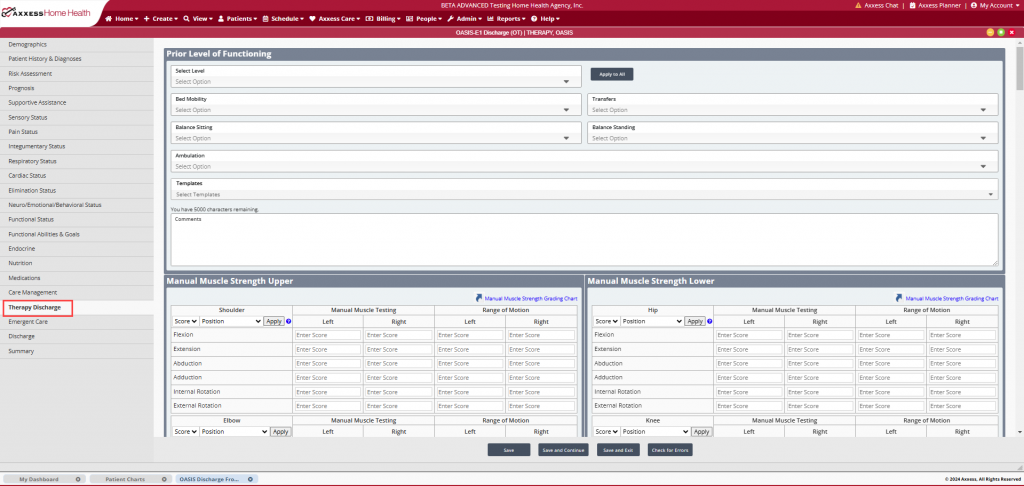
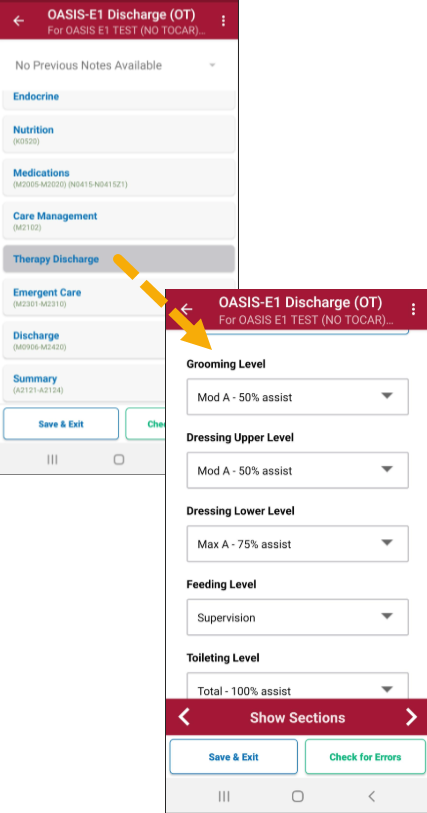
Therapy OASIS Updates
The therapy evaluation within the OASIS has been updated to better align with therapy assessments and evaluations. In addition, a Therapy Discharge tab has been added to the OASIS Discharge. This can be found under the Care Management tab.
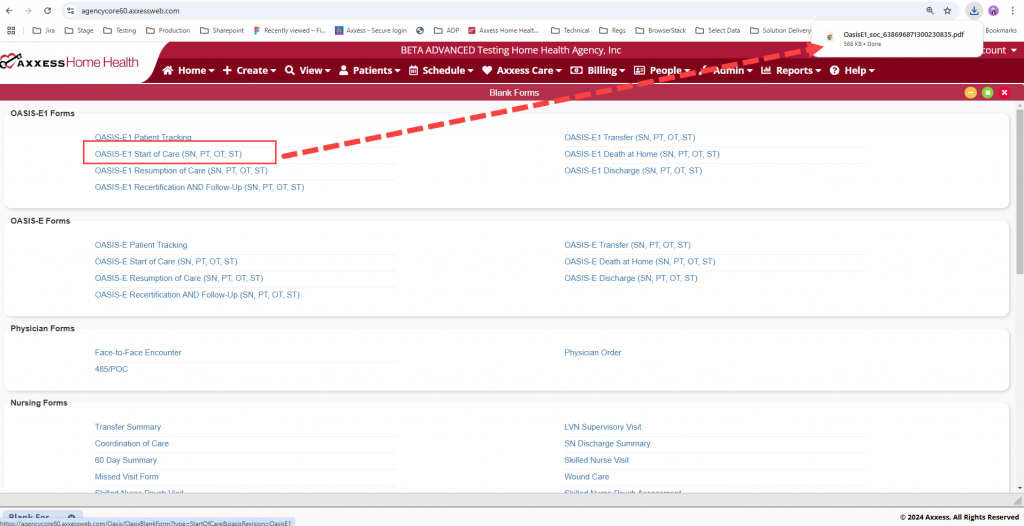
OASIS-E1 Blank Forms
Blank OASIS-E1 forms are available for download. To access the forms, navigate to the View tab, select Blank Forms from the drop-down menu, then select the desired form. The file will then download to the user’s device.
Updated on 12/18/2024